Since Rachel Reeves’ Budget, practices have been thinking hard about their team costs and pay structure, making plans for when the new National Insurance rules bite after April. To recap, the Employees’ NI rate remains the same, but the Employers’ rate rises to 15%; but the main additional costs come from the reduction in the threshold over which National Insurance is payable.
This has almost halved to £5,000, which means that almost all staff will fall within the grasp of Employers’ National Insurance. Practices where most of these staff are full-time will certainly notice the difference, with an extra £5,000 or so attracting the 15%, but this will be much more marked and a much bigger shock to those with a higher proportion of part-time staff.
As an example in the extreme, a practice with eight part-time staff each being paid £10,000 pa will have paid only minimal National Insurance in the past, but now will be paying for everyone.
Any business has a cost ‘personality’. It operates based on its habitual cost structure, cutting its cloth to fit the cash flows available. This ‘habit’ is not always easily nor immediately changeable. For practices with a higher proportion of part-time staff, this will give a severe jolt to its normal operating situation.
However, Rachel Reeves offered an offsetting benefit to businesses, being the increase in the annual allowance against PAYE/NIC given to employers. Does this offset the increased costs? We at DJH are fortunate enough to act for a sufficiently large number of practices to be able to examine a sample to assess the impact.
Without formally running through a statistics prism, we looked at practices ranging from a Gross income of £400,000 through to £1.2 m, with different mixtures of part-time and full-time staff in the team. On average, we found the additional cost due to the National Insurance increases to generally range between £650 and £850 per employee.
As expected, those with higher levels of part-time staff came off worse in the cost change. However, when we introduce the increased annual allowance, we found that this cost uplift was highly diluted so that the net increase came out much lower. For the smallest practices, the increase was wiped out; for the larger within our range, it was reduced to an additional around £100-300 per person.
As the allowance is essentially limited to a built-in maximum beyond which no further benefit is given, practices at the higher end of the range will save less per employee. Practices with higher Gross income than those we examined above, and therefore those, with larger payrolls, have less dilution, so will proportionally pay more.
But this is not the whole story of the cost increases. All suppliers will also been making similar decisions and potentially increasing their prices accordingly. In our analysis we have also considered which suppliers’ costs in an average dental practice may be affected and subject to a rise. Clearly this varies hugely, on size and geography as well as the principals’ modus operandi.
Very roughly, we conclude that, on average, a rise of 0.9 % of Gross turnover of a practice may not be unreasonable. In other words, for a practice with a Gross of £1m, they may need an anticipation for general overhead rises of £9,000 per annum. This cost increase sits on top of the direct staff costs increases, and of course depends on the size of the practice.
No account of the increase in minimum wage has been plotted in.
However: there is a very major exception to the benefit of the allowance increase. Practices working within the NHS are not allowed to claim it on the staff proportion utilised for NHS dentistry. To be blunt, NHS dentistry as it stands bears the whole brunt of the NI increases, both on their own staff and the indirect cost increases from their suppliers, with none of the offsetting allowance increase.
And of course, NHS practices are unable to increase their pricing to their patients in the same way as independent operators can. This is a double whammy. It does not need to be spelt out how this puts the words and intentions of the Health Secretary Wes Streeting directly in conflict with the Chancellor.
I would have thought that this anomaly, with the extreme threat and message that it carries to an NHS practitioner, would have been resolved by now, but it hasn't. It needs to be. The CDO is working hard on it, but it is the Treasury and the DoH which need to act. Practices are making decisions now with April in mind.
The closer we get to 5 April without reassurance to NHS GDPs, the more that practices fearful off the cost increase will decide to dump their NHS book. Now is the time for a decision and action to support and reassure NHS practitioners if the Government doesn’t want to lose another tranche of NHS access over the edge.
Enter your details above to receive a link you can use to download your FREE pdf
Read More

Here's What New Associates Need To Know
What Is Your Definition Of Retirement?

How Often Do You Look Back On Your Life And Think “I Wish That I Knew Than What I Know Now?”
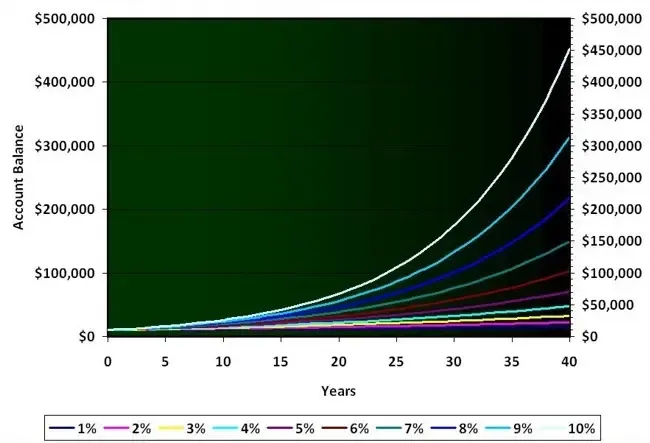
Can I Invest In My ISA For Passive Income?

The Role Of Luck In Investing